Avortament: diferència entre les revisions
| Línia 77: | Línia 77: | ||
Reported methods of unsafe, [[self-induced abortion]] include misuse of [[misoprostol]], and insertion of non-surgical implements such as knitting needles and clothes hangers into the uterus. These methods are rarely seen in developed countries where surgical abortion is legal and available.<ref>{{Cite journal |last1=Thapa |first1=S. R. |last2=Rimal |first2=D. |last3=Preston |first3=J. |title=Self induction of abortion with instrumentation |journal=Australian Family Physician |volume=35 |issue=9 |pages=697–698 |year=2006 |pmid=16969439| url=http://www.racgp.org.au/afp/200609/11015}}</ref> All of these, and any other method to terminate pregnancy may be called "induced miscarriage". |
Reported methods of unsafe, [[self-induced abortion]] include misuse of [[misoprostol]], and insertion of non-surgical implements such as knitting needles and clothes hangers into the uterus. These methods are rarely seen in developed countries where surgical abortion is legal and available.<ref>{{Cite journal |last1=Thapa |first1=S. R. |last2=Rimal |first2=D. |last3=Preston |first3=J. |title=Self induction of abortion with instrumentation |journal=Australian Family Physician |volume=35 |issue=9 |pages=697–698 |year=2006 |pmid=16969439| url=http://www.racgp.org.au/afp/200609/11015}}</ref> All of these, and any other method to terminate pregnancy may be called "induced miscarriage". |
||
{{clear}}<!-- The clr tag prevents the picture from running into the next section. Please keep it at the bottom of this section. --> |
{{clear}}<!-- The clr tag prevents the picture from running into the next section. Please keep it at the bottom of this section. --> |
||
==Seguretat== |
|||
[[Fitxer:Abortion Quick & Pain Free sign, Joe Slovo Park, Cape Town, South Africa-3869.jpg|thumb|right|Un pamflet d'avortament a Sud-àfrica]] |
|||
The health risks of abortion depend principally upon whether the procedure is performed safely or unsafely. The [[World Health Organization]] defines [[unsafe abortion]]s as those performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities.<ref name="who-unsafe-1995">{{cite web| publisher=[[World Health Organization]] |title=The Prevention and Management of Unsafe Abortion |date=April 1995| accessdate=1 June 2010 |url=http://whqlibdoc.who.int/hq/1992/WHO_MSM_92.5.pdf |format=PDF| archiveurl= https://web.archive.org/web/20100530072310/http://whqlibdoc.who.int/hq/1992/WHO_MSM_92.5.pdf| archivedate= 30 May 2010 | deadurl= no}}</ref> Legal abortions performed in the [[developed country|developed world]] are among the safest procedures in medicine.<ref name="lancet-grimes" /><ref name="grimes-overview">{{cite journal |last1=Grimes |first1=DA |last2=Creinin |first2=MD |title=Induced abortion: an overview for internists |journal=Ann. Intern. Med. |volume=140 |issue=8 |pages=620–6 |year=2004 |pmid=15096333 |doi= 10.7326/0003-4819-140-8-200404200-00009|url=http://www.annals.org/content/140/8/620.full}}</ref> In the US, the risk of [[mortality rate|maternal death]] from abortion is 0.7 per 100,000 procedures,<ref name="Ray2014" /> making abortion about 13 times safer for women than childbirth (8.8 maternal deaths per 100,000 live births).<ref name="grimes-mortality-2012">{{Cite journal| last1=Raymond |first1=E. G. |last2=Grimes |first2=D. A. |doi=10.1097/AOG.0b013e31823fe923 |title=The Comparative Safety of Legal Induced Abortion and Childbirth in the United States |journal=Obstetrics & Gynecology |volume=119 |issue=2, Part 1 |pages=215–219 |year=2012 |pmid=22270271 |pmc=}}</ref><ref name="grimes-mortality-2006">{{cite journal |author=Grimes DA |title=Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991 to 1999 |journal=Am. J. Obstet. Gynecol. |volume=194 |issue=1 |pages=92–4 |date=January 2006 |pmid=16389015 |doi=10.1016/j.ajog.2005.06.070 |url=}}</ref> The risk of abortion-related mortality increases with gestational age, but remains lower than that of childbirth through at least 21 weeks' gestation.<ref name="bartlett">{{cite journal |author=Bartlett LA |title=Risk factors for legal induced abortion-related mortality in the United States |journal=Obstet Gynecol |volume=103 |issue=4 |pages=729–37 |date=April 2004 |pmid=15051566 |doi=10.1097/01.AOG.0000116260.81570.60 |url= |author2=Berg CJ |author3=Shulman HB |last4=Zane |first4=Suzanne B. |last5=Green |first5=Clarice A. |last6=Whitehead |first6=Sara |last7=Atrash |first7=Hani K.|display-authors=3 }}</ref><ref name="emedicine">{{cite web |publisher=[[eMedicine]] |title=Elective Abortion |date=27 May 2010 |accessdate=1 June 2010 |first=Suzanne |last=Trupin |quote=At every gestational age, elective abortion is safer for the mother than carrying a pregnancy to term. |url=http://emedicine.medscape.com/article/252560-overview}}</ref><ref name="Genevra-2012">{{cite news|url=http://www.reuters.com/article/2012/01/23/us-abortion-idUSTRE80M2BS20120123|title=Abortion safer than giving birth: study|last=Pittman|first=Genevra |date=23 January 2012|publisher=Reuters|accessdate=4 February 2012}}</ref> Outpatient abortion is as safe and effective from 64 to 70 days' gestation as it is from 57 to 63 days.<ref>{{cite journal|last1=Abbas|first1=D|last2=Chong|first2=E|last3=Raymond|first3=EG|title=Outpatient medical abortion is safe and effective through 70 days gestation.|journal=Contraception|date=September 2015|volume=92|issue=3|pages=197–9|pmid=26118638|doi=10.1016/j.contraception.2015.06.018}}</ref> In the United States from 2000 to 2009, abortion had a lower mortality rate than [[plastic surgery]].<ref>{{cite journal|last1=Raymond|first1=EG|last2=Grossman|first2=D|last3=Weaver|first3=MA|last4=Toti|first4=S|last5=Winikoff|first5=B|title=Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States.|journal=Contraception|date=November 2014|volume=90|issue=5|pages=476–9|doi=10.1016/j.contraception.2014.07.012|pmid=25152259}}</ref> |
|||
[[Vacuum aspiration]] in the first trimester is the safest method of surgical abortion, and can be performed in a [[primary care|primary care office]], [[abortion clinic]], or hospital. Complications are rare and can include [[uterine perforation]], [[endometritis|pelvic infection]], and retained products of conception requiring a second procedure to evacuate.<ref name="arch-fam-practice">{{cite journal|vauthors=Westfall JM, Sophocles A, Burggraf H, Ellis S |title=Manual vacuum aspiration for first-trimester abortion |journal=Arch Fam Med |volume=7 |issue=6 |pages=559–62 |year=1998 |pmid=9821831 |doi=10.1001/archfami.7.6.559 |url=http://archfami.ama-assn.org/cgi/content/full/7/6/559 |deadurl=yes |archiveurl=https://web.archive.org/web/20050405202853/http://archfami.ama-assn.org/cgi/content/full/7/6/559 |archivedate=5 April 2005 }}</ref> Infections account for one-third of abortion-related deaths in the United States.<ref>{{cite journal|last1=Dempsey|first1=A|title=Serious infection associated with induced abortion in the United States.|journal=Clinical Obstetrics and Gynecology|date=December 2012|volume=55|issue=4|pages=888–92|doi=10.1097/GRF.0b013e31826fd8f8|pmid=23090457}}</ref> The rate of complications of vacuum aspiration abortion in the first trimester is similar regardless of whether the procedure is performed in a hospital, surgical center, or office.<ref>{{cite journal|last1=White|first1=Kari|last2=Carroll|first2=Erin|last3=Grossman|first3=Daniel|title=Complications from first-trimester aspiration abortion: a systematic review of the literature|journal=Contraception|date=November 2015|volume=92|issue=5|pages=422–438|doi=10.1016/j.contraception.2015.07.013|pmid=26238336}}</ref> Preventive antibiotics (such as [[doxycycline]] or [[metronidazole]]) are typically given before elective abortion,<ref>{{cite journal |title=ACOG practice bulletin No. 104: antibiotic prophylaxis for gynecologic procedures |journal=Obstet Gynecol |volume=113 |issue=5 |pages=1180–9 |date=May 2009 |pmid=19384149 |doi=10.1097/AOG.0b013e3181a6d011 |url= |author1= ACOG Committee on Practice Bulletins—Gynecology}}</ref> as they are believed to substantially reduce the risk of postoperative uterine infection.<ref name="NEJMDec2011" /><ref>{{cite journal |vauthors=Sawaya GF, Grady D, Kerlikowske K, Grimes DA |title=Antibiotics at the time of induced abortion: the case for universal prophylaxis based on a meta-analysis |journal=Obstet Gynecol |volume=87 |issue=5 Pt 2 |pages=884–90 |date=May 1996 |pmid=8677129 |doi= |url=}}</ref> The rate of failed procedures does not appear to vary significantly depending on whether the abortion is performed by a doctor or a [[mid-level practitioner]].<ref>{{cite journal|last1=Barnard|first1=S|last2=Kim|first2=C|last3=Park|first3=MH|last4=Ngo|first4=TD|title=Doctors or mid-level providers for abortion.|journal=The Cochrane Database of Systematic Reviews|date=27 July 2015|issue=7|pages=CD011242|doi=10.1002/14651858.CD011242.pub2|pmid=26214844}}</ref> Complications after second-trimester abortion are similar to those after first-trimester abortion, and depend somewhat on the method chosen. |
|||
There is little difference in terms of safety and efficacy between medical abortion using a combined regimen of mifepristone and misoprostol and surgical abortion (vacuum aspiration) in early first trimester abortions up to 9 weeks gestation.<ref name="WHO FAQs 2006"/> Medical abortion using the prostaglandin analog misoprostol alone is less effective and more painful than medical abortion using a combined regimen of mifepristone and misoprostol or surgical abortion.<ref>{{cite web|author=Grossman D|date=3 September 2004|title= Medical methods for first trimester abortion: RHL commentary|work=Reproductive Health Library|location=Geneva|publisher=World Health Organization|url=http://apps.who.int/rhl/fertility/abortion/dgcom/en/index.html |accessdate=22 November 2011}}</ref><ref>{{cite web|vauthors=Chien P, Thomson M |date=15 December 2006|title=Medical versus surgical methods for first trimester termination of pregnancy: RHL commentary|work=Reproductive Health Library|location=Geneva|publisher=World Health Organization|url=http://apps.who.int/rhl/fertility/abortion/pccom/en/index.html |accessdate=1 June 2010| archiveurl= https://web.archive.org/web/20100517201143/http://apps.who.int/rhl/fertility/abortion/pccom/en/index.html| archivedate= 17 May 2010 | deadurl= no}}</ref> |
|||
Some purported risks of abortion are promoted primarily by anti-abortion groups, but lack scientific support.<ref name="JASEN">{{cite journal |author=Jasen P |title=Breast cancer and the politics of abortion in the United States |journal=Med Hist |volume=49 |issue=4 |pages=423–44 |date=October 2005 |pmid=16562329 |pmc=1251638 |doi= 10.1017/S0025727300009145}}</ref> For example, the question of a [[abortion-breast cancer hypothesis|link between induced abortion and breast cancer]] has been investigated extensively. Major medical and scientific bodies (including the [[World Health Organization]], the US [[National Cancer Institute]], the [[American Cancer Society]], the [[Royal College of Obstetricians and Gynaecologists]] and the [[American Congress of Obstetricians and Gynecologists]]) have concluded that abortion does not cause breast cancer,<ref>Position statements of major medical bodies on abortion and breast cancer include: |
|||
* World Health Organization: {{cite web|url=http://www.who.int/mediacentre/factsheets/fs240/en/ |title=Induced abortion does not increase breast cancer risk (Fact sheet N°240) |publisher=World Health Organization |accessdate=6 January 2011 |archiveurl=https://web.archive.org/web/20110213141046/http://www.who.int/mediacentre/factsheets/fs240/en/ |archivedate=13 February 2011 }} |
|||
* National Cancer Institute: {{cite web|url=http://www.cancer.gov/cancertopics/factsheet/risk/abortion-miscarriage |title=Abortion, Miscarriage, and Breast Cancer Risk |publisher=National Cancer Institute |accessdate=11 January 2011 |archiveurl=https://web.archive.org/web/20101221084337/http://www.cancer.gov/cancertopics/factsheet/Risk/abortion-miscarriage |archivedate=21 December 2010 |deadurl=no }} |
|||
* American Cancer Society: {{cite web|url=http://www.cancer.org/Cancer/BreastCancer/MoreInformation/is-abortion-linked-to-breast-cancer |publisher=[[American Cancer Society]] |date=23 September 2010 |accessdate=20 June 2011 |title=Is Abortion Linked to Breast Cancer? |quote=At this time, the scientific evidence does not support the notion that abortion of any kind raises the risk of breast cancer. |archiveurl=https://web.archive.org/web/20110605204701/http://www.cancer.org/Cancer/BreastCancer/MoreInformation/is-abortion-linked-to-breast-cancer |archivedate=5 June 2011 |deadurl=no }} |
|||
* Royal College of Obstetricians and Gynaecologists: {{cite web|url=http://www.rcog.org.uk/files/rcog-corp/uploaded-files/NEBAbortionSummary.pdf |title=The Care of Women Requesting Induced Abortion |page=9 |format=PDF |publisher=Royal College of Obstetricians and Gynaecologists |accessdate=29 June 2008 |quote=Induced abortion is not associated with an increase in breast cancer risk. |deadurl=yes |archiveurl=https://web.archive.org/web/20130727105037/http://www.rcog.org.uk/files/rcog-corp/uploaded-files/NEBAbortionSummary.pdf |archivedate=27 July 2013 }} |
|||
* American Congress of Obstetricians and Gynecologists: {{cite web|url=http://www.acog.org/from_home/publications/press_releases/nr07-31-03-2.cfm |title=ACOG Finds No Link Between Abortion and Breast Cancer Risk |date=31 July 2003 |publisher=American Congress of Obstetricians and Gynecologists |accessdate=11 January 2011 |archiveurl=https://web.archive.org/web/20110102030744/http://www.acog.org/from_home/publications/press_releases/nr07-31-03-2.cfm |archivedate=2 January 2011 |deadurl=no }}</ref> although such a link continues to be studied<ref name="Lanfranchi2014">{{cite journal|author1=Lanfranchi, Angela|author2=Fagan, Patrick|title=Breast Cancer and Induced Abortion: A Comprehensive Review of Breast Development and Pathophysiology, the Epidemiologic Literature, and Proposal for Creation of Databanks to Elucidate All Breast Cancer Risk Factors|journal=Issues in Law & Medicine | date=2014 | volume=29 | issue=1 | pages=1–133 | url=http://www.bcpinstitute.org/papers/ILM_Vol%2029_No1_1-133.pdf | accessdate=11 November 2015 | quote=Given what is known of breast physiology, we can conclude that the following factors are protective, or decrease the likelihood that a woman will develop breast cancer: • Full-term pregnancy or pregnancy lasting longer than 32 weeks • Multiparity (more than one full-term pregnancy) • Short period (“susceptibility window”) between menarche and first full-term pregnancy • Full-term pregnancy soon after abortion or second-trimester miscarriage • Breastfeeding}}</ref><ref name=Huang_meta_analysis_2014>{{cite journal | author1=Huang Yubei | author2=Zhang Xiaoliang | title=A meta-analysis of the association between induced abortion and breast cancer risk among Chinese females | journal=Cancer Causes Control | date=February 2014 | volume=25 | issue=2 | pages=227–236 | doi=10.1007/s10552-013-0325-7 | pmid=24272196 | url=http://static-content.springer.com/esm/art%3A10.1007%2Fs10552-013-0325-7/MediaObjects/10552_2013_325_MOESM1_ESM.pptx | accessdate=11 November 2015 | publisher=Springer International Publishing | issn=1573-7225 | quote=Compared to people without any history of [induced abortion], an increased risk of breast cancer was observed among females who had at least one [induced abortion]. | display-authors=etal}}</ref> and promoted by anti-abortion groups.<ref name="JASEN"/><ref name=Cancer_Linacre>{{cite journal|author1=Schneider, A. Patrick II|author2=Zainer, Christine|title=The breast cancer epidemic: 10 facts|journal=The Linacre Quarterly|date=August 2014|volume=81|issue=3|pages=244–277|doi=10.1179/2050854914Y.0000000027|url=http://www.maneyonline.com/doi/full/10.1179/2050854914Y.0000000027|accessdate=11 November 2015|publisher=Catholic Medical Association|quote=...an association between [induced abortion] and breast cancer has been found by numerous Western and non-Western researchers from around the world. This is especially true in more recent reports that allow for a sufficient breast cancer latency period since an adoption of a Western life style in sexual and reproductive behavior.|display-authors=etal|doi-access=free}}</ref> |
|||
===Salut mental=== |
|||
{{AP|Avortament i salut mental}} |
|||
There is no relationship between most induced abortions and [[abortion and mental health|mental-health problems]]<ref name=BMJ2014/><ref name="Cockburn">{{Cite book|last1=Cockburn|first1=Jayne |last2=Pawson|first2=Michael E. |title=Psychological Challenges to Obstetrics and Gynecology: The Clinical Management |year=2007 |publisher=Springer |isbn=978-1-84628-807-4 |page=243}}</ref> other than those expected for any unwanted pregnancy.<ref name="apa-press"/> The [[American Psychological Association]] has concluded that a woman's first abortion is not a threat to mental health when carried out in the first trimester, with such women no more likely to have mental-health problems than those carrying an unwanted pregnancy to term; the mental-health outcome of a woman's second or greater abortion is less certain.<ref name="apa-press">{{cite press release |publisher=[[American Psychological Association]] |title=APA Task Force Finds Single Abortion Not a Threat to Women's Mental Health |date=12 August 2008 |accessdate=7 September 2011 |url=http://www.apa.org/news/press/releases/2008/08/single-abortion.aspx}}</ref><ref>{{cite web|url=http://www.apa.org/pi/women/programs/abortion/mental-health.pdf |title=Report of the APA Task Force on Mental Health and Abortion |publisher=[[American Psychological Association]] |location=Washington, DC |date=13 August 2008}}</ref> Although some studies show negative mental-health outcomes in women who choose abortions after the first trimester because of fetal abnormalities,<ref name="apa-2008">{{cite web | url = http://www.apa.org/pi/women/programs/abortion/index.aspx | title = Mental Health and Abortion | publisher = [[American Psychological Association]] | year = 2008 | accessdate = 18 April 2012}}</ref> more rigorous research would be needed to show this conclusively.<ref name="Steinberg2011">{{Cite journal |last1=Steinberg |first1=J. R. |title=Later Abortions and Mental Health: Psychological Experiences of Women Having Later Abortions—A Critical Review of Research |doi=10.1016/j.whi.2011.02.002 |journal=Women's Health Issues |volume=21 |issue=3 |pages=S44–S48 |year=2011 |pmid=21530839}}</ref> Some proposed negative psychological effects of abortion have been referred to by anti-abortion advocates as a separate condition called "[[post-abortion syndrome]]", which is not recognized by medical or psychological professionals in the United States.<ref>{{cite journal|last1=Kelly|first1=Kimberly|title=The spread of ‘Post Abortion Syndrome’ as social diagnosis|journal=Social Science & Medicine|date=February 2014|volume=102|pages=18–25|doi=10.1016/j.socscimed.2013.11.030}}</ref> |
|||
===Avortament insegur=== |
|||
{{AP|Avortament insegur}} |
|||
[[File:RussianAbortionPoster.jpg|thumb|Soviet poster circa 1925, warning against midwives performing abortions. Title translation: "Abortions performed by either trained or self-taught midwives not only maim the woman, they also often lead to death."]] |
|||
Women seeking to terminate their pregnancies sometimes resort to unsafe methods, particularly when access to legal abortion is restricted. They may attempt to [[self-induced abortion|self-abort]] or rely on another person who does not have proper medical training or access to proper facilities. This has a tendency to lead to severe complications, such as incomplete abortion, [[sepsis]], hemorrhage, and damage to internal organs.<ref>{{Cite journal|last1=Okonofua |first1=F. |title=Abortion and maternal mortality in the developing world |journal=Journal of Obstetrics and Gynaecology Canada |volume=28 |issue=11 |pages=974–979 |year=2006 |pmid=17169222 |url=http://www.jogc.org/abstracts/full/200611_WomensHealth_1.pdf |format=PDF |deadurl=yes |archiveurl=https://web.archive.org/web/20120111121431/http://www.jogc.org/abstracts/full/200611_WomensHealth_1.pdf |archivedate=11 January 2012 |df=dmy }}</ref> |
|||
Unsafe abortions are a major cause of injury and death among women worldwide. Although data are imprecise, it is estimated that approximately 20 million unsafe abortions are performed annually, with 97% taking place in [[developing country|developing countries]].<ref name="lancet-grimes"/> Unsafe abortions are believed to result in millions of injuries.<ref name="lancet-grimes"/><ref name="Haddad-2009">{{Cite journal|last1=Haddad |first1=LB. |last2=Nour |first2=NM. |title=Unsafe abortion: unnecessary maternal mortality |journal=Rev Obstet Gynecol |volume=2 |issue=2 |pages=122–6|year=2009 |doi=|pmid=19609407 |pmc=2709326}}</ref> Estimates of deaths vary according to methodology, and have ranged from 37,000 to 70,000 in the past decade;<ref name="lancet-grimes"/><ref name=OBGY09/><ref name=Loz2012>{{cite journal|last=Lozano|first=R|title=Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010.|journal=Lancet|date=15 December 2012|volume=380|issue=9859|pages=2095–128|pmid=23245604|doi=10.1016/S0140-6736(12)61728-0|hdl=10536/DRO/DU:30050819|hdl-access=free}}</ref> deaths from unsafe abortion account for around 13% of all [[maternal deaths]].<ref>{{cite book|last=Darney|first=Leon Speroff, Philip D.|title=A clinical guide for contraception|year=2010|publisher=Lippincott Williams & Wilkins|location=Philadelphia, Pa.|isbn=1-60831-610-6|page=406|edition=5th }}</ref> The [[World Health Organization]] believes that mortality has fallen since the 1990s.<ref name="WHO2011">{{cite book|last=World Health Organisation|title=Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008 |publisher=World Health Organisation |year=2011 |edition=6th |page=27 |isbn=978-92-4-150111-8 |url=http://whqlibdoc.who.int/publications/2011/9789241501118_eng.pdf |format=PDF}}</ref> To reduce the number of unsafe abortions, public health organizations have generally advocated emphasizing the legalization of abortion, training of medical personnel, and ensuring access to reproductive-health services.<ref name="berer-who">{{cite journal |author=Berer M |title=Making abortions safe: a matter of good public health policy and practice |journal=Bull. World Health Organ. |volume=78 |issue=5 |pages=580–92 |year=2000 |pmid=10859852 |pmc=2560758}}</ref> However, the Dublin Declaration on Maternal Health, signed in 2012, notes that "the prohibition of abortion does not affect, in any way, the availability of optimal care to pregnant women".<ref>{{cite web | url =http://www.dublindeclaration.com/translations/|title=Translations|publisher=Dublin Declaration| accessdate =28 October 2015}}</ref> |
|||
A major factor in whether abortions are performed safely or not is the legal standing of abortion. Countries with restrictive abortion laws have higher rates of unsafe abortion and similar overall abortion rates compared to those where abortion is legal and available.<ref name="OBGY09"/><ref name="Sedgh 2012"/><ref name="berer-who"/><ref name="Sedgh 2007">{{cite journal |vauthors=Sedgh G, Henshaw S, Singh S, Ahman E, Shah IH |title =Induced abortion: estimated rates and trends worldwide |year=2007 |journal=Lancet |volume=370 |issue=9595 |pages=1338–45 |doi=10.1016/S0140-6736(07)61575-X |pmid=17933648|citeseerx=10.1.1.454.4197 }}</ref><ref name="WHO-unsafe-2007">{{cite web |publisher=[[World Health Organization]] |year=2007 |accessdate=7 March 2011 |format=PDF |url=http://whqlibdoc.who.int/publications/2007/9789241596121_eng.pdf |title=Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003 |archiveurl= https://web.archive.org/web/20110216141018/http://whqlibdoc.who.int/publications/2007/9789241596121_eng.pdf| archivedate= 16 February 2011 |deadurl= no}}</ref><ref>{{cite journal |author=Berer M |title=National laws and unsafe abortion: the parameters of change |journal=Reprod Health Matters |volume=12 |issue=24 Suppl |pages=1–8 |date=November 2004 |pmid=15938152 |doi= 10.1016/S0968-8080(04)24024-1|url=}}</ref><ref>{{cite journal|last1=Culwell|first1=Kelly R.|last2=Hurwitz|first2=Manuelle|title=Addressing barriers to safe abortion|journal=International Journal of Gynecology & Obstetrics|date=May 2013|volume=121|pages=S16–S19|doi=10.1016/j.ijgo.2013.02.003}}</ref> For example, the 1996 legalization of abortion in South Africa had an immediate positive impact on the frequency of abortion-related complications,<ref name="jewkes">{{cite journal |vauthors=Jewkes R, Rees H, Dickson K, Brown H, Levin J |title=The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change |journal=BJOG |volume=112 |issue=3 |pages=355–9 |date=March 2005 |pmid=15713153 |doi=10.1111/j.1471-0528.2004.00422.x |url=}}</ref> with abortion-related deaths dropping by more than 90%.<ref name="bateman-samj">{{cite journal |author=Bateman C |title=Maternal mortalities 90% down as legal TOPs more than triple |journal=S. Afr. Med. J. |volume=97 |issue=12 |pages=1238–42 |date=December 2007 |pmid=18264602}}</ref> Similar reductions in maternal mortality have been observed after other countries have liberalized their abortion laws, such as [[Romania]] and [[Nepal]].<ref>{{cite journal|last1=Conti|first1=Jennifer A.|last2=Brant|first2=Ashley R.|last3=Shumaker|first3=Heather D.|last4=Reeves|first4=Matthew F.|title=Update on abortion policy|journal=[[Current Opinion in Obstetrics and Gynecology]]|date=November 2016|pages=1|doi=10.1097/GCO.0000000000000324}}</ref> A 2011 study concluded that in the United States, some state-level anti-abortion laws are correlated with lower rates of abortion in that state.<ref>{{cite journal|last1=New|first1=M. J.|title=Analyzing the Effect of Anti-Abortion U.S. State Legislation in the Post-Casey Era|journal=State Politics & Policy Quarterly|date=15 February 2011|volume=11|issue=1|pages=28–47|doi=10.1177/1532440010387397}}</ref> The analysis, however, did not take into account travel to other states without such laws to obtain an abortion.<ref>{{cite journal|last1=Medoff|first1=M. H.|last2=Dennis|first2=C.|title=Another Critical Review of New's Reanalysis of the Impact of Antiabortion Legislation|journal=State Politics & Policy Quarterly|date=21 July 2014|volume=14|issue=3|pages=269–276|doi=10.1177/1532440014535476}}</ref> In addition, a lack of access to effective contraception contributes to unsafe abortion. It has been estimated that the incidence of unsafe abortion could be reduced by up to 75% (from 20 million to 5 million annually) if modern family planning and maternal health services were readily available globally.<ref name="Singh">{{cite web|url=http://www.guttmacher.org/pubs/FB-AIU-summary.pdf |title=Facts on Investing in Family Planning and Maternal and Newborn Health |format=PDF |publisher=[[Guttmacher Institute]] |year=2010 |accessdate=24 May 2012 |deadurl=yes |archiveurl=https://web.archive.org/web/20120324101905/http://www.guttmacher.org/pubs/FB-AIU-summary.pdf |archivedate=24 March 2012 }}</ref> Rates of such abortions may be difficult to measure because they can be reported variously as miscarriage, "induced miscarriage", "menstrual regulation", "mini-abortion", and "regulation of a delayed/suspended menstruation".<ref name=Pandemic>{{cite web |url=http://www.who.int/reproductivehealth/publications/unsafe_abortion/lancet_paper/en/ |
|||
|title = Unsafe Abortion - The Preventable Pandemic* |
|||
|accessdate = 2010-01-16 |
|||
|last = Grimes |
|||
|first = David A.}}</ref><ref name=Brazil_Unsafe>{{cite journal|last1=Nations|first1=MK|title=Women’s hidden transcripts about abortion in Brazil|journal=Soc Sci Med|date=1997|volume=44|pages=1833–45|doi=10.1016/s0277-9536(96)00293-6|pmid=9194245}}</ref> |
|||
Forty percent of the world's women are able to access therapeutic and elective abortions within gestational limits,<ref name="IJGO10"/> while an additional 35 percent have access to legal abortion if they meet certain physical, mental, or socioeconomic criteria.<ref name="Dev98-07"/> While [[maternal death|maternal mortality]] seldom results from safe abortions, unsafe abortions result in 70,000 deaths and 5 million disabilities per year.<ref name=OBGY09/> Complications of unsafe abortion account for approximately an eighth of [[maternal death|maternal mortalities]] worldwide,<ref name="Maclean">{{cite book|last=Maclean|first=Gaynor|url=https://books.google.com/books?id=u4Aeiu2eDMAC&pg=PA299|chapter=XI. Dimension, Dynamics and Diversity: A 3D Approach to Appraising Global Maternal and Neonatal Health Initiatives|pages=299–300|title=Trends in Midwifery Research|editor1-first=Randell E.|editor1-last=Balin|publisher=Nova Publishers|year=2005|isbn=978-1-59454-477-4}}</ref> though this varies by region.<ref>{{cite journal|author=Salter, C. |author2=Johnson, H.B. |author3=Hengen, N. |year=1997 |url=http://info.k4health.org/pr/l10edsum.shtml |title=Care for Postabortion Complications: Saving Women's Lives |journal=Population Reports |volume=25 |issue=1 |publisher=Johns Hopkins School of Public Health |archiveurl=https://web.archive.org/web/20091207070103/http://info.k4health.org/pr/l10edsum.shtml |dead-url=yes |archivedate=7 December 2009 |df= }}</ref> Secondary infertility caused by an unsafe abortion affects an estimated 24 million women.<ref name="WHO-unsafe-2007"/> The rate of unsafe abortions has increased from 44% to 49% between 1995 and 2008.<ref name="Sedgh 2012" /> Health education, access to family planning, and improvements in health care during and after abortion have been proposed to address this phenomenon.<ref>{{cite web|title=Packages of interventions: Family planning, safe abortion care, maternal, newborn and child health|authors=[[UNICEF]], [[United Nations Population Fund]], WHO, World Bank |year=2010 |accessdate=31 December 2010|url=http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/fch_10_06/en/index.html}}</ref> |
|||
===Nascut viu=== |
|||
Although it is very uncommon, women undergoing surgical abortion after 18 weeks gestation sometimes give birth to a fetus that may survive briefly.<ref name=RCOG_2nd-trimester>{{cite journal|title=The Care of Women Requesting Induced Abortion. Evidence-Based Clinical Guideline no. 7|journal=Royal College of Obstetricians and Gynaecologists|date=November 2011|url=https://www.rcog.org.uk/globalassets/documents/guidelines/abortion-guideline_web_1.pdf|accessdate=31 October 2015|quote=RECOMMENDATION 6.21 Feticide should be performed before medical abortion after 21 weeks and 6 days of gestation to ensure that there is no risk of a live birth.}}</ref><ref name=Labor_Induced_Abortionb>{{cite journal|last1=Society of Family Planning|title=Clinical Guidelines, Labor induction abortion in the second trimester|journal=Contraception|date=February 2011|volume=84|issue=1|pages=4–18|doi=10.1016/j.contraception.2011.02.005|url=http://www.contraceptionjournal.org/article/S0010-7824(11)00057-6/pdf|quote="Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin."}}</ref><ref name=Fletcher_Ethics>{{cite journal|author1=Fletcher|author2=Isada|author3=Johnson|author4=Evans|title=Fetal intracardiac potassium chloride injection to avoid the hopeless resuscitation of an abnormal abortus: II. Ethical issues.|journal=Obstetrics and Gynecology|date=Aug 1992|volume=80|issue=2|pages=310–313|pmid=1635751|quote="... following later abortions at greater than 20 weeks, the rare but catastrophic occurrence of live births can lead to fractious controversy over neonatal management."}}</ref> [[Fetal viability|Longer term survival]] is possible after 22 weeks.<ref name=RCOG_Term>{{cite journal|title=Termination of Pregnancy for Fetal Abnormality|journal=Royal College of Obstetricians and Gynaecologists|date=May 2010|pages=29–31|url=https://www.rcog.org.uk/globalassets/documents/guidelines/terminationpregnancyreport18may2010.pdf|accessdate=26 October 2015}}</ref> |
|||
If medical staff observe signs of life, they may be required to provide care: emergency medical care if the child has a good chance of survival and palliative care if not.<ref name=Nuffield_Bioethics>{{cite journal|last1=Nuffield Council on Bioethics|title=Critical care decisions in fetal and neonatal medicine: a guide to the report|date=2007|url=http://nuffieldbioethics.org/wp-content/uploads/2014/07/CCD-Short-Version-FINAL.pdf|accessdate=29 October 2015|quote=Under English law, fetuses have no independent legal status. Once born, babies have the same rights to life as other people.}}</ref><ref name=US_Ethics>{{cite journal|author1=Gerri R. Baer|author2=Robert M. Nelson|title=Preterm Birth: Causes, Consequences, and Prevention. C: A Review of Ethical Issues Involved in Premature Birth|journal=Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes;|date=2007|url=http://www.ncbi.nlm.nih.gov/books/NBK11389/|quote=In 2002, the 107th U.S. Congress passed the Born-Alive Infants Protection Act of 2001. This law established personhood for all infants who are born “at any stage of development” who breathe, have a heartbeat, or “definite movement of voluntary muscles,” regardless of whether the birth was due to labor or induced abortion.}}</ref><ref name=BAIPA>{{cite web|last1=Chabot|first1=Steve|title=H.R. 2175 (107th): Born-Alive Infants Protection Act of 2002|url=https://www.govtrack.us/congress/bills/107/hr2175|website=govtrack.us|accessdate=30 October 2015|ref=Pub.L. 107-207|date=5 August 2002|quote=The term ``born alive is defined as the complete expulsion or extraction from its mother of that member, at any stage of development, who after such expulsion or extraction breathes or has a beating heart, pulsation of the umbilical cord, or definite movement of the voluntary muscles, regardless of whether the umbilical cord has been cut, and regardless of whether the expulsion or extraction occurs as a result of natural or induced labor, cesarean section, or induced abortion.}}</ref> [[feticide#Use during legal abortion|Induced fetal demise]] before termination of pregnancy after 20–21 weeks gestation is recommended to avoid this.<ref name=ACOG_2nd>{{cite journal|title=Practice Bulletin: Second-Trimester Abortion|journal=Obstetrics & Gynecology|date=June 2013|volume=121|issue=6|pages=1394–1406|doi=10.1097/01.AOG.0000431056.79334.cc|pmid=23812485|url=http://blog.utp.edu.co/maternoinfantil/files/2012/04/135-Aborto-2-trimestre.pdf|accessdate=30 October 2015|quote=With medical abortion after 20 weeks of gestation, induced fetal demise may be preferable to the woman or provider in order to avoid transient fetal survival after expulsion.}}</ref><ref name=SFP_Demise>{{cite journal|title=Clinical Guidelines: Induction of fetal demise before abortion|journal=Contraception: a publication of Society of Family Planning|date=January 2010|page=8|doi=10.1016/j.contraception.2010.01.018|url=http://www.societyfp.org/_documents/resources/InductionofFetalDemise.pdf|quote="Inducing fetal demise before induction termination avoids signs of live birth that may have beneficial emotional, ethical and legal consequences."|accessdate=26 October 2015|volume=81}}</ref><ref name=ACOG_demise>{{cite journal|last1=Committee on Health Care for Underserved Women|title=Committee Opinion 613: Increasing Access to Abortion|journal=Obstetrics & Gynecology|date=November 2014|volume=124|pages=1060–1065|url=http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Increasing-Access-to-Abortion?IsMobileSet=false|accessdate=28 October 2015|quote=“Partial-birth” abortion bans—The federal Partial-Birth Abortion Ban Act of 2003 (upheld by the Supreme Court in 2007) makes it a federal crime to perform procedures that fall within the definition of so-called “partial-birth abortion” contained in the statute, with no exception for procedures necessary to preserve the health of the woman...physicians and lawyers have interpreted the banned procedures as including intact dilation and evacuation unless fetal demise occurs before surgery.|doi=10.1097/01.aog.0000456326.88857.31}}</ref><ref name=NAF_2015>{{cite journal|title=2015 Clinical Policy Guidelines|journal=National Abortion Federation|date=2015|url=http://prochoice.org/wp-content/uploads/2015_NAF_CPGs.pdf|accessdate=30 October 2015|quote=Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.}}</ref><ref name=FIGO_Ethical>{{cite journal|title=FIGO (International Federation of Gynecology and Obstetrics) Committee Report: Ethical aspects concerning termination of pregnancy following prenatal diagnosis.|journal=International Journal of Gynecology and Obstetrics|quote="Termination of pregnancy following prenatal diagnosis after 22 weeks must be preceded by a feticide"|date=2008|issue=1|pages=97–98|doi=10.1016/j.ijgo.2008.03.002|pmid=18423641|volume=102}}</ref> |
|||
Death following live birth which is caused by abortion is given the [[ICD-10 Chapter XVI: Certain conditions originating in the perinatal period#(P90–P96) Other disorders originating in the perinatal period|ICD-10 underlying cause description code of P96.4]]; data are identified as either fetus or newborn. Between 1999 and 2013, in the U.S., the [[Centers for Disease Control and Prevention|CDC]] recorded 531 such deaths for newborns,<ref name=CDC_ICD-10_P96.4_Newborn>{{cite journal|title=Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015|journal=Centers for Disease Control and Prevention, National Center for Health Statistics|url=http://wonder.cdc.gov/ucd-icd10.html|accessdate=12 November 2015|location=Data are from the Multiple Cause of Death Files, 1999-2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program}}</ref> approximately 4 per 100,000 abortions.<ref name=CDC_Surveillance_2006>{{cite journal|last1=Pazol|first1=Karen|title=Abortion Surveillance - United States, 2006|journal=Morbidity and Mortality Weekly Report Surveillance Summaries|date=27 November 2009|volume=58|issue=SS08|pages=1–35|url=http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5808a1.htm?s_cid=ss5808a1_e|accessdate=12 November 2015|display-authors=etal}}</ref> |
|||
== Avortament en animals == |
== Avortament en animals == |
||
Revisió del 00:27, 7 juny 2017
|
|
Aquest article o secció s'està elaborant i està inacabat. Un viquipedista hi està treballant i és possible que trobeu defectes de contingut o de forma. Comenteu abans els canvis majors per coordinar-los. Aquest avís és temporal: es pot treure o substituir per {{incomplet}} després d'uns dies d'inactivitat. |

L'avortament és un terme mèdic per designar la interrupció de l'embaràs per l'expulsió del fetus abans que aquest sigui viable entre les 20 i les 28 setmanes.[1][2] Pot ser espontani o induït. L'avortament espontani és la pèrdua del fetus sense cap intervenció humana. Pot ser accidental (per una infecció, un trauma, una intoxicació, un defecte del fetus…) en una persona que ja ha tingut embarassos normals, o habitual (regular) quan una malformació, un defecte hormonal o alguna altra causa impossibilita que el fetus pugui créixer normalment. L'avortament induït o avortament provocat resulta de les accions empreses amb la intenció d'interrompre l'embaràs.
Es parla d'avortament terapèutic, quan, entre d'altres la continuació de l'embaràs o el part signifiquen un risc greu per a la vida de la mare, per evitar el naixement d'un nen amb una malaltia congènita o genètica greu fatal o que el condemna a patiments o discapacitats molt greus, o per reduir el nombre de fetus en embarassos múltiples fins a un nombre que faci el risc acceptable.
En el cas d'embaràs no desitjat, es pot provocar l'avortament, quan la dona decideix que no pot o no vol tenir l'infant per raons personals, socials, psicològiques o de salut mental. Aquests criteris poden ser legítims o no segons el marc legal corresponent. Practicat per professionals de la salut habilitats i completat quan necessari per suport psicològic i social, el risc de complicacions sanitàries o psicosocials és mínim.[3][4] Aquesta forma d'avortament provocat sovint és matèria de controvèrsia ètica i de restriccions legals. Als països de la Unió Europea està autoritzat, dins els límits de la llei.
L'avortament clandestí, en ser executat per no sanitaris, sovint sense unes mesures d'higiene apropiades, o sense una preparació o un seguiment adequats, és una de les principals causes de mort en dones joves, particularment en els països menys desenvolupats. En total, cada any moren unes 70.000 dones per aquest motiu, particularment a Àsia, on es produeix el 55% dels avortaments clandestins.[5]
Sobre problemes sexuals i d'embaràs no desitjat, a Catalunya es pot recórrer als Centres d'Atenció Primària, amb Atenció a la Salut Sexual i Reproductiva (ASSIR).[6]
Tipus
Segons les causes de l'avortament, es poden distingir dos tipus:
Induït
Aproximadament 205 milions d'embarassos es donen cada any en tot el món. Al voltant d'una tercera part són no desitjats i al voltant d'una cinquena part acaben en abort induït.[7][8] La major part dels avortaments resulten d'embarassos no desitjats.[9][10] Al Regne Unit, de l'1 al 2% dels avortaments són conseqüència de problemes genètics en el fetus.[11] Un embaràs es pot interrompre intenciodament de diferents maneres. La manera que es selecciona depèn sovint de l'edat de gestació de l'embrió o el fetus, que augmenta en mida a mesura que l'embaràs progressa.[12][13] També es poden seleccionar procesdiments específics segons legalitat, disponibilitat regional o preferència personal del doctor o del pacient.
Les raons per a les quals es produeix un avortament induït es caracteritzen típicament com terapèutiques o electives. Un avortament és referit en termes mèdics com un avortament terapèutic quan es fa per tal de salvar la vida de la dona embarassada; evitar dolor físic o mental a la dona; finalitzar un embaràs en què segons les indicacions el nadó tindrà una alta esperança de morbiditat prematura, mortalitat o altrament discapacitat; o la reducció selectiva del nombre de fetus per reduir riscos sanitaris associats a l'embaràs múltiple.[14][15] Es considera que un avortament és electiu o voluntari quan es dóna per sol·licitud de la dona per raons no mèdiques.[15] Sovint hi ha confusió al voltant del terme "electiu" perquè la cirurgia electiva es refereix generalment a tota cirurgia programada que no suposa una emergència, ja sigui necessària en termes mèdics o no.[16]
Espontani
L'avortament espontani, és l'expulsió no intencional de l'embrió o fetus abans de la 24a setmana de gestació.[17] L'embaràs que acaba abans de les 37 setmanes de gestació resultant en un naixement es coneix com a part preterme o part prematur[18] Quan un fetus mor in utero després de la viabilitat fetal o durant el treball de part, s'anomenen habitualment mort fetal.[19] Es diu que no hi ha viabilitat fetal quan el fetus té un pes menor a 500 grams o quan l'avortament espontani es produeix abans de les 20 setmanes de gestació. Els naixements prematurs i les morts fetals no es consideren generalment avortaments espontanis tot i que l'ús d'aquests termes els pot confondre de vegades.[20]
Només del 30% al 50% de les concepcions progressen més enllà del primer trimestre.[21] L'àmplia majoria d'aquests que no progressen es perden abans que la dona sigui conscient de la concepció,[15] i molts embarassos es perden abans que els mèdics clínics puguin detectar l'embrió.[22] El 80% d'aquests avortaments espontanis passen en el primer trimestre.[23] La causa més comuna de l'avortament espontani durant el primer trimestre és la mutació cromosòmica de l'embrió o del fetus,[15][24] que es dóna en almenys un 50% de les pèrdues analitzades en aquest període.[25] Altres causes inclouen malalties vasculars (com ara el lupus), la diabetis, altres problemes hormonalas, infeccions, i anormalitats de l'úter.[24] L'edat avançada de la mare o l'historial d'avortaments espontanis previs són els dos factors principals associats a un risc més gran de contraure avortament espontani.[25] Un avortament espontani també pot ser causat per un trauma físic; un trauma intencional o l'estrés com a causa d'avortament espontani es poden considerar avortament induït o feticidi.[26] L'avortament espontani es classifica en precoç, si es produeix abans de la dotzena setmana de gestació; i tardà, quan es produeix entre les setmanes 12 i 22 de gestació.
Mètodes
Mèdic
Els avortaments mèdics són els induïts per abortius farmacèutics. L'avortament mèdic es va convertir en un mètode alternatiu d'avortament amb la disponibilitat de anàlegs de Prostaglandina els anys 1970 i la mifepristona antiprogestàgen (també coneguda com a RU-486) els anys 1980.[27][28][29][30][31]
El règim més comú de principis del primer trimestre d'avortament mèdic s'usa la mifepristona en combinació amb un anàleg de les prostaglandina (misoprostol o gemeprost) fins a 9 setmanes d'edat gestacional, metotrexat en combinació amb una anàleg de prostaglandina fins a 7 setmanes de gestació, o un anàleg de la prostaglandina sola.[29] Els règims de combinació de mifepristona–misoprostol treballen més ràpid i són més eficaços en edats gestacionals més tard que els règims de combinació de metotrexat i misoprostol, i els règims de combinació són més eficaços que el misoprostol sol.[30] Aquest règim és efectiu en el segon trimestre.[32] Els regiments d'avortaments mèdics que impliquen la mifepristona seguida de misoprostol entre 24 i 48 hores més tard són eficaços quan es realitza abans de 63 dies de gestació.[33]
En avortaments molt primerencs, de fins a 7 setmanes de gestació, l'avortament mèdic usant un règim de combinació de mifepristona-misoprostol es considera que és més eficaç que l'avortament quirúrgic (aspiració per buit), especialment quan la pràctica clínica no inclou inspecció detallada de teixit aspirat.[34] Els primers règims d'avortament mèdic usant mifepristona, seguit de 24-48 hores més tard per misoprostol bucal o vaginal són un 98% eficaços fins a 9 setmanes d'edat gestacional.[35] Si l'avortament mèdic falla, ha de ser utilitzat l'avortament quirúrgic per completar el procediment.[36]
Els avortaments mèdics primerencs representen la majoria dels avortaments abans de les 9 setmanes de gestació a la Gran Bretanya,[37][38] França,[39] Suïssa,[40] i els països nòrdics.[41] Als Estats Units, el percentatge d'avortaments mèdics primerencs és molt menor.[42][43]
Els règims d'avortament amb medicaments utilitzant mifepristona en combinació amb un anàleg de les prostaglandines són els mètodes més comuns utilitzats per avortaments del segon trimestre al Canadà, la major part d'Europa, la Xina i l'Índia,[31] en contrast amb els Estats Units, on el 96% d'avortaments del segon trimestre es realitzen quirúrgicament per la dilatació i evacuació.[44]
Quirúrgic
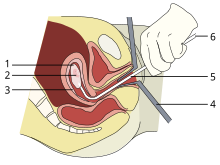
1: Sac amniòtic
2: Embrió
3: Revestiment uterí
4: Espècul
5: Vacurette
6: Unida a una bomba de succió
Fins a 15 setmanes de gestació, la succió-aspiració o aspiració al buit són els mètodes quirúrgics més comuns d'avortament induït.[45] El Manual vacuum aspiration (MVA, en català: aspiració de buit manual) consisteix en l'eliminació del fetus o l'embrió, placenta, i membranes per succió usant una xeringa manual, mentre que electric vacuum aspiration (EVA, en català: aspiració de buit elèctrica) utilitza una bomba elèctrica. Aquestes tècniques difereixen en el mecanisme utilitzat per aplicar el buit, en què tan d'hora en l'embaràs que poden ser utilitzats, i en si és necessària la dilatació cervical.
MVA, also known as "mini-suction" and "menstrual extraction", can be used in very early pregnancy, and does not require cervical dilation. Dilation and curettage (D&C), the second most common method of surgical abortion, is a standard gynecological procedure performed for a variety of reasons, including examination of the uterine lining for possible malignancy, investigation of abnormal bleeding, and abortion. Curettage refers to cleaning the walls of the uterus with a curette. The World Health Organization recommends this procedure, also called sharp curettage, only when MVA is unavailable.[46]
From the 15th week of gestation until approximately the 26th, other techniques must be used. Dilation and evacuation (D&E) consists of opening the cervix of the uterus and emptying it using surgical instruments and suction. After the 16th week of gestation, abortions can also be induced by intact dilation and extraction (IDX) (also called intrauterine cranial decompression), which requires surgical decompression of the fetus's head before evacuation. IDX is sometimes called "partial-birth abortion", which has been federally banned in the United States.
In the third trimester of pregnancy, induced abortion may be performed surgically by intact dilation and extraction or by hysterotomy. Hysterotomy abortion is a procedure similar to a caesarean section and is performed under general anesthesia. It requires a smaller incision than a caesarean section and is used during later stages of pregnancy.[47]
First-trimester procedures can generally be performed using local anesthesia, while second-trimester methods may require deep sedation or general anesthesia.[43]
Avortament per inducció del part
In places lacking the necessary medical skill for dilation and extraction, or where preferred by practitioners, an abortion can be induced by first inducing labor and then inducing fetal demise if necessary.[48] This is sometimes called "induced miscarriage". This procedure may be performed from 13 weeks gestation to the third trimester. Although it is very uncommon in the United States, more than 80% of induced abortions throughout the second trimester are labor induced abortions in Sweden and other nearby countries.[49]
Only limited data are available comparing this method with dilation and extraction.[49] Unlike D&E, labor induced abortions after 18 weeks may be complicated by the occurrence of brief fetal survival, which may be legally characterized as live birth. For this reason, labor induced abortion is legally risky in the U.S.[49][50]
Altres mètodes
Historically, a number of herbs reputed to possess abortifacient properties have been used in folk medicine: tansy, pennyroyal, black cohosh, and the now-extinct silphium.[51] The use of herbs in such a manner can cause serious—even lethal—side effects, such as multiple organ failure, and is not recommended by physicians.[52]
Abortion is sometimes attempted by causing trauma to the abdomen. The degree of force, if severe, can cause serious internal injuries without necessarily succeeding in inducing miscarriage.[53] In Southeast Asia, there is an ancient tradition of attempting abortion through forceful abdominal massage.[54] One of the bas reliefs decorating the temple of Angkor Wat in Cambodia depicts a demon performing such an abortion upon a woman who has been sent to the underworld.[54]
Reported methods of unsafe, self-induced abortion include misuse of misoprostol, and insertion of non-surgical implements such as knitting needles and clothes hangers into the uterus. These methods are rarely seen in developed countries where surgical abortion is legal and available.[55] All of these, and any other method to terminate pregnancy may be called "induced miscarriage".
Seguretat

The health risks of abortion depend principally upon whether the procedure is performed safely or unsafely. The World Health Organization defines unsafe abortions as those performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities.[56] Legal abortions performed in the developed world are among the safest procedures in medicine.[57][58] In the US, the risk of maternal death from abortion is 0.7 per 100,000 procedures,[59] making abortion about 13 times safer for women than childbirth (8.8 maternal deaths per 100,000 live births).[60][61] The risk of abortion-related mortality increases with gestational age, but remains lower than that of childbirth through at least 21 weeks' gestation.[62][63][64] Outpatient abortion is as safe and effective from 64 to 70 days' gestation as it is from 57 to 63 days.[65] In the United States from 2000 to 2009, abortion had a lower mortality rate than plastic surgery.[66]
Vacuum aspiration in the first trimester is the safest method of surgical abortion, and can be performed in a primary care office, abortion clinic, or hospital. Complications are rare and can include uterine perforation, pelvic infection, and retained products of conception requiring a second procedure to evacuate.[67] Infections account for one-third of abortion-related deaths in the United States.[68] The rate of complications of vacuum aspiration abortion in the first trimester is similar regardless of whether the procedure is performed in a hospital, surgical center, or office.[69] Preventive antibiotics (such as doxycycline or metronidazole) are typically given before elective abortion,[70] as they are believed to substantially reduce the risk of postoperative uterine infection.[43][71] The rate of failed procedures does not appear to vary significantly depending on whether the abortion is performed by a doctor or a mid-level practitioner.[72] Complications after second-trimester abortion are similar to those after first-trimester abortion, and depend somewhat on the method chosen.
There is little difference in terms of safety and efficacy between medical abortion using a combined regimen of mifepristone and misoprostol and surgical abortion (vacuum aspiration) in early first trimester abortions up to 9 weeks gestation.[34] Medical abortion using the prostaglandin analog misoprostol alone is less effective and more painful than medical abortion using a combined regimen of mifepristone and misoprostol or surgical abortion.[73][74]
Some purported risks of abortion are promoted primarily by anti-abortion groups, but lack scientific support.[75] For example, the question of a link between induced abortion and breast cancer has been investigated extensively. Major medical and scientific bodies (including the World Health Organization, the US National Cancer Institute, the American Cancer Society, the Royal College of Obstetricians and Gynaecologists and the American Congress of Obstetricians and Gynecologists) have concluded that abortion does not cause breast cancer,[76] although such a link continues to be studied[77][78] and promoted by anti-abortion groups.[75][79]
Salut mental
There is no relationship between most induced abortions and mental-health problems[11][80] other than those expected for any unwanted pregnancy.[81] The American Psychological Association has concluded that a woman's first abortion is not a threat to mental health when carried out in the first trimester, with such women no more likely to have mental-health problems than those carrying an unwanted pregnancy to term; the mental-health outcome of a woman's second or greater abortion is less certain.[81][82] Although some studies show negative mental-health outcomes in women who choose abortions after the first trimester because of fetal abnormalities,[83] more rigorous research would be needed to show this conclusively.[84] Some proposed negative psychological effects of abortion have been referred to by anti-abortion advocates as a separate condition called "post-abortion syndrome", which is not recognized by medical or psychological professionals in the United States.[85]
Avortament insegur
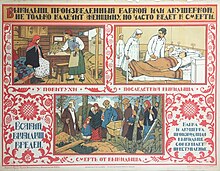
Women seeking to terminate their pregnancies sometimes resort to unsafe methods, particularly when access to legal abortion is restricted. They may attempt to self-abort or rely on another person who does not have proper medical training or access to proper facilities. This has a tendency to lead to severe complications, such as incomplete abortion, sepsis, hemorrhage, and damage to internal organs.[86]
Unsafe abortions are a major cause of injury and death among women worldwide. Although data are imprecise, it is estimated that approximately 20 million unsafe abortions are performed annually, with 97% taking place in developing countries.[57] Unsafe abortions are believed to result in millions of injuries.[57][87] Estimates of deaths vary according to methodology, and have ranged from 37,000 to 70,000 in the past decade;[57][88][89] deaths from unsafe abortion account for around 13% of all maternal deaths.[90] The World Health Organization believes that mortality has fallen since the 1990s.[91] To reduce the number of unsafe abortions, public health organizations have generally advocated emphasizing the legalization of abortion, training of medical personnel, and ensuring access to reproductive-health services.[92] However, the Dublin Declaration on Maternal Health, signed in 2012, notes that "the prohibition of abortion does not affect, in any way, the availability of optimal care to pregnant women".[93]
A major factor in whether abortions are performed safely or not is the legal standing of abortion. Countries with restrictive abortion laws have higher rates of unsafe abortion and similar overall abortion rates compared to those where abortion is legal and available.[88][7][92][94][95][96][97] For example, the 1996 legalization of abortion in South Africa had an immediate positive impact on the frequency of abortion-related complications,[98] with abortion-related deaths dropping by more than 90%.[99] Similar reductions in maternal mortality have been observed after other countries have liberalized their abortion laws, such as Romania and Nepal.[100] A 2011 study concluded that in the United States, some state-level anti-abortion laws are correlated with lower rates of abortion in that state.[101] The analysis, however, did not take into account travel to other states without such laws to obtain an abortion.[102] In addition, a lack of access to effective contraception contributes to unsafe abortion. It has been estimated that the incidence of unsafe abortion could be reduced by up to 75% (from 20 million to 5 million annually) if modern family planning and maternal health services were readily available globally.[103] Rates of such abortions may be difficult to measure because they can be reported variously as miscarriage, "induced miscarriage", "menstrual regulation", "mini-abortion", and "regulation of a delayed/suspended menstruation".[104][105]
Forty percent of the world's women are able to access therapeutic and elective abortions within gestational limits,[106] while an additional 35 percent have access to legal abortion if they meet certain physical, mental, or socioeconomic criteria.[107] While maternal mortality seldom results from safe abortions, unsafe abortions result in 70,000 deaths and 5 million disabilities per year.[88] Complications of unsafe abortion account for approximately an eighth of maternal mortalities worldwide,[108] though this varies by region.[109] Secondary infertility caused by an unsafe abortion affects an estimated 24 million women.[95] The rate of unsafe abortions has increased from 44% to 49% between 1995 and 2008.[7] Health education, access to family planning, and improvements in health care during and after abortion have been proposed to address this phenomenon.[110]
Nascut viu
Although it is very uncommon, women undergoing surgical abortion after 18 weeks gestation sometimes give birth to a fetus that may survive briefly.[111][112][113] Longer term survival is possible after 22 weeks.[114]
If medical staff observe signs of life, they may be required to provide care: emergency medical care if the child has a good chance of survival and palliative care if not.[115][116][117] Induced fetal demise before termination of pregnancy after 20–21 weeks gestation is recommended to avoid this.[118][119][120][121][122]
Death following live birth which is caused by abortion is given the ICD-10 underlying cause description code of P96.4; data are identified as either fetus or newborn. Between 1999 and 2013, in the U.S., the CDC recorded 531 such deaths for newborns,[123] approximately 4 per 100,000 abortions.[124]
Avortament en animals
Avortament espontani
Els animals no humans també poden patir avortaments espontanis. En el cas de les vaques, per exemple, hi ha diversos factors que poden interrompre la gestació, incloent-hi el consum de plantes verinoses i les infeccions.[125] S'han relacionat els desequilibris de vitamina A, vitamina E, seleni i ferro, així com les temperatures elevades i els traumatismes, amb la pèrdua de fetus.[126] Les causes d'avortament en les ovelles són similars. A vegades resulta difícil diagnosticar l'avortament en aquestes dues espècies.[127]
Referències
- ↑ «Avortament induït o provocat: causes, procediments i possibles conseqüències». Wikinotícia, 10 desembre 2004 [Consulta: d'octubre 2014].
- ↑ «Avortament». Gran Enciclopèdia Catalana. Barcelona: Grup Enciclopèdia Catalana.
- ↑ «Abortion and the safety of women» (en anglès). BBC Ethics Guide, 2014 [Consulta: 8 novembre 2014].
- ↑ Major, Brenda; et al.. APA Task Force on Mental Health and Abortion. Mental Health and Abortion (pdf) (en anglès). American Psychological Association, 2008, p. 105.
- ↑ «Mueren 70.000 mujeres cada año por abortos clandestinos» (en castellà). Direcció d'Obra Social per al Personal Universitari de la Universitat Nacional de San Luis, 08-09-2004.
- ↑ «Atenció a la salut sexual i reproductiva (ASSIR)». Institut Català de la Salut, 15-04-2014. [Consulta: 9 gener 2016].
- ↑ 7,0 7,1 7,2 Sedgh, G.; Singh, S.; Shah, I. H.; Åhman, E.; Henshaw, S. K.; Bankole, A. «Induced abortion: Incidence and trends worldwide from 1995 to 2008» (PDF). The Lancet, 379, 9816, 2012, pàg. 625–632. DOI: 10.1016/S0140-6736(11)61786-8. PMID: 22264435. «Com que poques de les estimacions d'avortament es basaven en estudis de mostres aleatòries de dones, i com que no vam usar una aproximació basada en cap model per estimar la incidència de l'avortament, no va ser possible calcular intervals de confiança basats en l'error estàndard sobre les aproximacions. A partir de la informació accessible en l'exactitud i la precisió en les estimacions de l'avortament que es van usar per desenvolupar taxes regional, subregionals i globals, vam calcular intervals de certesa al voltant d'aquestes taxes (webappendix). Vam calcular intervals més amplis per taxes d'avortament poc segur que en tazes d'avortament segur.»
- ↑ Cheng L. «Surgical versus medical methods for second-trimester induced abortion». The WHO Reproductive Health Library. World Health Organization, 01-11-2008. Arxivat de l'original el 17 juny 2011. [Consulta: 17 juny 2011].
- ↑ Bankole; etal «Reasons Why Women Have Induced Abortions: Evidence from 27 Countries». International Family Planning Perspectives, 24, 3, 1998, pàg. 117–127 & 152. DOI: 10.2307/3038208.
- ↑ Finer, Lawrence B.; Frohwirth, Lori F.; Dauphinee, Lindsay A.; Singh, Susheela; Moore, Ann M. «Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives» (PDF). Perspectives on Sexual and Reproductive Health, 37, 3, 2005, pàg. 110–118. DOI: 10.1111/j.1931-2393.2005.tb00045.x. PMID: 16150658.
- ↑ 11,0 11,1 Lohr, PA; Fjerstad, M; Desilva, U; Lyus, R «Abortion». BMJ, 348, 2014, pàg. f7553. DOI: 10.1136/bmj.f7553.
- ↑ Stubblefield, Phillip G. «10. Family Planning». A: Novak's Gynecology. 13. Lippincott Williams & Wilkins, 2002. ISBN 978-0-7817-3262-8.
- ↑ Bartlett, LA; Berg, CJ; Shulman, HB; Zane, SB «Risk factors for legal induced abortion-related mortality in the United States». Obstetrics & Gynecology, 103, 4, 2004, p. 729–37. DOI: 10.1097/01.AOG.0000116260.81570.60.
- ↑ Roche, Natalie E. «Therapeutic Abortion». eMedicine, 28-09-2004. Arxivat de l'original el 14 desembre 2004. [Consulta: 19 juny 2011].
- ↑ 15,0 15,1 15,2 15,3 «6. First-Trimester Abortion». A: Williams Gynecology. 1. McGraw-Hill Medical, 2008. ISBN 978-0-07-147257-9.
- ↑ «Elective surgery». Encyclopedia of Surgery. [Consulta: 17 desembre 2012]. "An elective surgery is a planned, non-emergency surgical procedure. It may be either medically required (e.g., cataract surgery), or optional (e.g., breast augmentation or implant) surgery.
- ↑ Churchill Livingstone medical dictionary. Edinburgh New York: Churchill Livingstone Elsevier, 2008. ISBN 978-0-443-10412-1. «En anglès el terme que es prefereix per la pèrdua no intencional del producte de la concepció abans de la 24a setmana és "miscarriage".»
- ↑ Annas, George J.; Elias, Sherman. «51. Legal and Ethical Issues in Obstetric Practice». A: Obstetrics: Normal and Problem Pregnancies. 5. Churchill Livingstone, 2007, p. 669. ISBN 978-0-443-06930-7. «A preterm birth is defined as one that occurs before the completion of 37 menstrual weeks of gestation, regardless of birth weight.»
- ↑ «Stillbirth». A: . Oxford University Press, 2010. «birth of a fetus that shows no evidence of life (heartbeat, respiration, or independent movement) at any time later than 24 weeks after conception»
- ↑ «7 FAM 1470 Documenting Stillbirth (Fetal Death)». United States Department of State, 18-02-2011. [Consulta: 12 gener 2016].
- ↑ Annas, George J.; Elias, Sherman. «24. Pregnancy loss». A: Obstetrics: Normal and Problem Pregnancies. 5. Churchill Livingstone, 2007. ISBN 978-0-443-06930-7.
- ↑ Katz, Vern L. «16. Spontaneous and Recurrent Abortion – Etiology, Diagnosis, Treatment». A: Katz: Comprehensive Gynecology. 5. Mosby, 2007. ISBN 978-0-323-02951-3.
- ↑ Williams Obstetrics. 24th. McGraw Hill Education, 2014. ISBN 978-0-07-179893-8.
- ↑ 24,0 24,1 Stöppler, Melissa Conrad. «Miscarriage (Spontaneous Abortion)». MedicineNet.com. WebMD. Arxivat de l'original el 29 agost 2004. [Consulta: 7 abril 2009].
- ↑ 25,0 25,1 Jauniaux E, Kaminopetros P, El-Rafaey H. «Early pregnancy loss». A: Whittle MJ, Rodeck CH. Fetal medicine: basic science and clinical practice. Edinburgh: Churchill Livingstone, 1999, p. 837. ISBN 978-0-443-05357-3. OCLC 42792567.
- ↑ «Fetal Homicide Laws». National Conference of State Legislatures. Arxivat de l'original el 29 març 2009. [Consulta: 7 abril 2009].
- ↑ Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenades1st_Methods - ↑ Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadesKapp2013 - ↑ 29,0 29,1 «Medical methods for first trimester abortion». Cochrane Database Syst Rev, vol. 11, 11, 2011, pàg. CD002855. DOI: 10.1002/14651858.CD002855.pub4. PMID: 22071804.
- ↑ 30,0 30,1 «Medical abortion in early pregnancy». A: Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell, 2009, p. 111–134. ISBN 1-4051-7696-2.
- ↑ 31,0 31,1 «Medical methods to induce abortion in the second trimester». A: Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell, 2009, p. 178–192. ISBN 1-4051-7696-2.
- ↑ Wildschut, H «Medical methods for mid-trimester termination of pregnancy.». Cochrane database of systematic reviews (Online), 1, 19-01-2011, pàg. CD005216. DOI: 10.1002/14651858.CD005216.pub2. PMID: 21249669.
- ↑ Chen, MJ; Creinin, MD «Mifepristone With Buccal Misoprostol for Medical Abortion: A Systematic Review.». Obstetrics and Gynecology, vol. 126, 1, July 2015, pàg. 12–21. DOI: 10.1097/AOG.0000000000000897. PMID: 26241251.
- ↑ 34,0 34,1 WHO Department of Reproductive Health and Research. Frequently asked clinical questions about medical abortion. Geneva: World Health Organization, 23 November 2006. ISBN 92-4-159484-5 [Consulta: 22 novembre 2011].(subscripció necessària)
- ↑ «Effectiveness of medical abortion with mifepristone and buccal misoprostol through 59 gestational days». Contraception, vol. 80, 3, September 2009, pàg. 282–286. DOI: 10.1016/j.contraception.2009.03.010. PMC: 3766037. PMID: 19698822. El règim (200 mg de mifepristona, seguit de 24-48 hores més tard per 800 mcg de misoprostol vaginal) prèviament usat per les clíniques Planned Parenthood als Estats Units des del 2001 al març de 2006 va ser un 98,5% efectiu a través dels 63 dies de gestació—amb una taxa d'embaràs en curs d'al voltant de 0,5% i un 1% addicional de dones que tenen l'evacuació uterina per diverses raons, incloent sagnat problemàtic, persistent sac gestacional, el judici clínic o una petició de la dona. El règim (200 mg de mifepristona, seguit de 24-48 hores més tard per 800 mcg de misoprostol buccal ) actualment usat per les clíniques Planned Parenthood als Estats Units des de l'abril de 2006 és un 98,3% efectiu a través de 59 dies de gestació.
- ↑ «Induced abortion». A: Danforth's obstetrics and gynecology. 10th. Philadelphia: Lippincott Williams & Wilkins, 2008, p. 586–603. ISBN 978-0-7817-6937-2.
- ↑ «Abortion statistics, England and Wales: 2010». London: Department of Health, United Kingdom, 24-05-2011. [Consulta: 22 novembre 2011].[Enllaç no actiu]
- ↑ «Abortion statistics, year ending 31 December 2010». Edinburgh: ISD, NHS Scotland, 31-05-2011. [Consulta: 22 novembre 2011].
- ↑ «Voluntary terminations of pregnancies in 2008 and 2009». Paris: DREES, Ministry of Health, France, 22-06-2011. Arxivat de l'original el 26 September 2011. [Consulta: 22 novembre 2011].
- ↑ .. «Abortions in Switzerland 2010». Neuchâtel: Office of Federal Statistics, Switzerland, 05-07-2011. [Consulta: 22 novembre 2011].
- ↑ «Induced abortions in the Nordic countries 2009». Helsinki: National Institute for Health and Welfare, Finland, 21-02-2011. [Consulta: 22 novembre 2011].
- ↑ «Abortion incidence and access to services in the United States, 2008». Perspect Sex Reprod Health, vol. 43, 1, March 2011, pàg. 41–50. DOI: 10.1363/4304111. PMID: 21388504 [Consulta: 22 novembre 2011].
- ↑ 43,0 43,1 43,2 Templeton, A.; Grimes, D. A. «A Request for Abortion». New England Journal of Medicine, vol. 365, 23, 2011, pàg. 2198–2204. DOI: 10.1056/NEJMcp1103639.
- ↑ «Dilation and evacuation». A: Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell, 2009, p. 178–192. ISBN 1-4051-7696-2.
- ↑ Healthwise. «Manual and vacuum aspiration for abortion». WebMD, 2004. Arxivat de l'original el 11 February 2007. [Consulta: 5 December 2008].
- ↑ World Health Organization. «Dilatation and curettage». A: Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva: World Health Organization, 2003. ISBN 978-92-4-154587-7. OCLC 181845530 [Consulta: 5 December 2008].
- ↑ McGee, Glenn. «Abortion». A: Encarta. Microsoft [Consulta: 5 December 2008].
- ↑ Borgatta, L «Labor Induction Termination of Pregnancy». Global Library of Women's Medicine, vol. GLOWM.10444, December 2014. DOI: 10.3843/GLOWM.10444 [Consulta: 25 setembre 2015].
- ↑ 49,0 49,1 49,2 Society of Family Planning «Clinical Guidelines, Labor induction abortion in the second trimester». Contraception, vol. 84, 1, February 2011, pàg. 4–18. DOI: 10.1016/j.contraception.2011.02.005 [Consulta: 25 setembre 2015]. «"10. What is the effect of feticide on labor induction abortion outcome? Deliberately causing demise of the fetus before labor induction abortion is performed primarily to avoid transient fetal survival after expulsion; this approach may be for the comfort of both the woman and the staff, to avoid futile resuscitation efforts. Some providers allege that feticide also facilitates delivery, although little data support this claim. Transient fetal survival is very unlikely after intraamniotic installation of saline or urea, which are directly feticidal. Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin. Factors associated with a higher likelihood of transient fetal survival with labor induction abortion include increasing gestational age, decreasing abortion interval and the use of nonfeticidal inductive agents such as the PGE1 analogues."»
- ↑ «2015 Clinical Policy Guidelines». National Abortion Federation, 2015 [Consulta: 30 octubre 2015]. «Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.»
- ↑ Riddle, John M. Eve's herbs: a history of contraception and abortion in the West. Cambridge, Massachusetts: Harvard University Press, 1997. ISBN 978-0-674-27024-4. OCLC 36126503.
- ↑ «Herbal infusions used for induced abortion». J. Toxicol. Clin. Toxicol., vol. 41, 3, 2003, pàg. 235–239. DOI: 10.1081/CLT-120021104. PMID: 12807304.
- ↑ Smith JP «Risky choices: The dangers of teens using self-induced abortion attempts». Journal of Pediatric Health Care, vol. 12, 3, 1998, pàg. 147–151. DOI: 10.1016/S0891-5245(98)90245-0. PMID: 9652283.
- ↑ 54,0 54,1 Potts, M.; Graff, M.; Taing, J. «Thousand-year-old depictions of massage abortion». Journal of Family Planning and Reproductive Health Care, vol. 33, 4, 2007, pàg. 233–234. DOI: 10.1783/147118907782101904. PMID: 17925100.
- ↑ Thapa, S. R.; Rimal, D.; Preston, J. «Self induction of abortion with instrumentation». Australian Family Physician, vol. 35, 9, 2006, pàg. 697–698. PMID: 16969439.
- ↑ «The Prevention and Management of Unsafe Abortion» (PDF). World Health Organization, April 1995. Arxivat de l'original el 30 May 2010. [Consulta: 1r juny 2010].
- ↑ 57,0 57,1 57,2 57,3 Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadeslancet-grimes - ↑ Grimes, DA; Creinin, MD «Induced abortion: an overview for internists». Ann. Intern. Med., vol. 140, 8, 2004, pàg. 620–6. DOI: 10.7326/0003-4819-140-8-200404200-00009. PMID: 15096333.
- ↑ Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadesRay2014 - ↑ Raymond, E. G.; Grimes, D. A. «The Comparative Safety of Legal Induced Abortion and Childbirth in the United States». Obstetrics & Gynecology, vol. 119, 2, Part 1, 2012, pàg. 215–219. DOI: 10.1097/AOG.0b013e31823fe923. PMID: 22270271.
- ↑ Grimes DA «Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991 to 1999». Am. J. Obstet. Gynecol., vol. 194, 1, January 2006, pàg. 92–4. DOI: 10.1016/j.ajog.2005.06.070. PMID: 16389015.
- ↑ Bartlett LA; Zane, Suzanne B.; Green, Clarice A.; Whitehead, Sara; Atrash, Hani K. «Risk factors for legal induced abortion-related mortality in the United States». Obstet Gynecol, vol. 103, 4, April 2004, pàg. 729–37. DOI: 10.1097/01.AOG.0000116260.81570.60. PMID: 15051566.
- ↑ Trupin, Suzanne. «Elective Abortion». eMedicine, 27-05-2010. [Consulta: 1r juny 2010]. «At every gestational age, elective abortion is safer for the mother than carrying a pregnancy to term.»
- ↑ Pittman, Genevra «Abortion safer than giving birth: study». Reuters, 23-01-2012 [Consulta: 4 febrer 2012].
- ↑ Abbas, D; Chong, E; Raymond, EG «Outpatient medical abortion is safe and effective through 70 days gestation.». Contraception, vol. 92, 3, September 2015, pàg. 197–9. DOI: 10.1016/j.contraception.2015.06.018. PMID: 26118638.
- ↑ Raymond, EG; Grossman, D; Weaver, MA; Toti, S; Winikoff, B «Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States.». Contraception, vol. 90, 5, November 2014, pàg. 476–9. DOI: 10.1016/j.contraception.2014.07.012. PMID: 25152259.
- ↑ «Manual vacuum aspiration for first-trimester abortion». Arch Fam Med, vol. 7, 6, 1998, pàg. 559–62. DOI: 10.1001/archfami.7.6.559. PMID: 9821831.
- ↑ Dempsey, A «Serious infection associated with induced abortion in the United States.». Clinical Obstetrics and Gynecology, vol. 55, 4, December 2012, pàg. 888–92. DOI: 10.1097/GRF.0b013e31826fd8f8. PMID: 23090457.
- ↑ White, Kari; Carroll, Erin; Grossman, Daniel «Complications from first-trimester aspiration abortion: a systematic review of the literature». Contraception, vol. 92, 5, November 2015, pàg. 422–438. DOI: 10.1016/j.contraception.2015.07.013. PMID: 26238336.
- ↑ «ACOG practice bulletin No. 104: antibiotic prophylaxis for gynecologic procedures». Obstet Gynecol, vol. 113, 5, May 2009, pàg. 1180–9. DOI: 10.1097/AOG.0b013e3181a6d011. PMID: 19384149.
- ↑ «Antibiotics at the time of induced abortion: the case for universal prophylaxis based on a meta-analysis». Obstet Gynecol, vol. 87, 5 Pt 2, May 1996, pàg. 884–90. PMID: 8677129.
- ↑ Barnard, S; Kim, C; Park, MH; Ngo, TD «Doctors or mid-level providers for abortion.». The Cochrane Database of Systematic Reviews, 7, 27-07-2015, pàg. CD011242. DOI: 10.1002/14651858.CD011242.pub2. PMID: 26214844.
- ↑ Grossman D. «Medical methods for first trimester abortion: RHL commentary». Reproductive Health Library. Geneva: World Health Organization, 03-09-2004. [Consulta: 22 novembre 2011].
- ↑ «Medical versus surgical methods for first trimester termination of pregnancy: RHL commentary». Reproductive Health Library. Geneva: World Health Organization, 15 December 2006. Arxivat de l'original el 17 May 2010. [Consulta: 1r juny 2010].
- ↑ 75,0 75,1 Jasen P «Breast cancer and the politics of abortion in the United States». Med Hist, vol. 49, 4, October 2005, pàg. 423–44. DOI: 10.1017/S0025727300009145. PMC: 1251638. PMID: 16562329.
- ↑ Position statements of major medical bodies on abortion and breast cancer include:
- World Health Organization: «Induced abortion does not increase breast cancer risk (Fact sheet N°240)». World Health Organization. Arxivat de l'original el 13 February 2011. [Consulta: 6 gener 2011].
- National Cancer Institute: «Abortion, Miscarriage, and Breast Cancer Risk». National Cancer Institute. Arxivat de l'original el 21 December 2010. [Consulta: 11 gener 2011].
- American Cancer Society: «Is Abortion Linked to Breast Cancer?». American Cancer Society, 23-09-2010. Arxivat de l'original el 5 June 2011. [Consulta: 20 juny 2011]. «At this time, the scientific evidence does not support the notion that abortion of any kind raises the risk of breast cancer.»
- Royal College of Obstetricians and Gynaecologists: «The Care of Women Requesting Induced Abortion» (PDF). Royal College of Obstetricians and Gynaecologists. Arxivat de l'original el 27 July 2013. [Consulta: 29 juny 2008]. «Induced abortion is not associated with an increase in breast cancer risk.»
- American Congress of Obstetricians and Gynecologists: «ACOG Finds No Link Between Abortion and Breast Cancer Risk». American Congress of Obstetricians and Gynecologists, 31-07-2003. Arxivat de l'original el 2 January 2011. [Consulta: 11 gener 2011].
- ↑ «Breast Cancer and Induced Abortion: A Comprehensive Review of Breast Development and Pathophysiology, the Epidemiologic Literature, and Proposal for Creation of Databanks to Elucidate All Breast Cancer Risk Factors». Issues in Law & Medicine, vol. 29, 1, 2014, pàg. 1–133 [Consulta: 11 novembre 2015]. «Given what is known of breast physiology, we can conclude that the following factors are protective, or decrease the likelihood that a woman will develop breast cancer: • Full-term pregnancy or pregnancy lasting longer than 32 weeks • Multiparity (more than one full-term pregnancy) • Short period (“susceptibility window”) between menarche and first full-term pregnancy • Full-term pregnancy soon after abortion or second-trimester miscarriage • Breastfeeding»
- ↑ «A meta-analysis of the association between induced abortion and breast cancer risk among Chinese females». Cancer Causes Control. Springer International Publishing, vol. 25, 2, February 2014, pàg. 227–236. DOI: 10.1007/s10552-013-0325-7. ISSN: 1573-7225. PMID: 24272196 [Consulta: 11 novembre 2015]. «Compared to people without any history of [induced abortion], an increased risk of breast cancer was observed among females who had at least one [induced abortion].»
- ↑ «The breast cancer epidemic: 10 facts». The Linacre Quarterly. Catholic Medical Association, vol. 81, 3, August 2014, pàg. 244–277. DOI: 10.1179/2050854914Y.0000000027 [Consulta: 11 novembre 2015]. «...an association between [induced abortion] and breast cancer has been found by numerous Western and non-Western researchers from around the world. This is especially true in more recent reports that allow for a sufficient breast cancer latency period since an adoption of a Western life style in sexual and reproductive behavior.»
- ↑ Cockburn, Jayne; Pawson, Michael E. Psychological Challenges to Obstetrics and Gynecology: The Clinical Management. Springer, 2007, p. 243. ISBN 978-1-84628-807-4.
- ↑ 81,0 81,1 American Psychological Association (12 August 2008). "APA Task Force Finds Single Abortion Not a Threat to Women's Mental Health". Nota de premsa. Consulta: 7 September 2011.
- ↑ «Report of the APA Task Force on Mental Health and Abortion». Washington, DC: American Psychological Association, 13-08-2008.
- ↑ «Mental Health and Abortion». American Psychological Association, 2008. [Consulta: 18 abril 2012].
- ↑ Steinberg, J. R. «Later Abortions and Mental Health: Psychological Experiences of Women Having Later Abortions—A Critical Review of Research». Women's Health Issues, vol. 21, 3, 2011, pàg. S44–S48. DOI: 10.1016/j.whi.2011.02.002. PMID: 21530839.
- ↑ Kelly, Kimberly «The spread of ‘Post Abortion Syndrome’ as social diagnosis». Social Science & Medicine, vol. 102, February 2014, pàg. 18–25. DOI: 10.1016/j.socscimed.2013.11.030.
- ↑ Okonofua, F. «Abortion and maternal mortality in the developing world» (PDF). Journal of Obstetrics and Gynaecology Canada, vol. 28, 11, 2006, pàg. 974–979. PMID: 17169222.
- ↑ Haddad, LB.; Nour, NM. «Unsafe abortion: unnecessary maternal mortality». Rev Obstet Gynecol, vol. 2, 2, 2009, pàg. 122–6. PMC: 2709326. PMID: 19609407.
- ↑ 88,0 88,1 88,2 Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadesOBGY09 - ↑ Lozano, R «Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010.». Lancet, vol. 380, 9859, 15 December 2012, pàg. 2095–128. DOI: 10.1016/S0140-6736(12)61728-0. PMID: 23245604.
- ↑ Darney, Leon Speroff, Philip D.. A clinical guide for contraception. 5th. Philadelphia, Pa.: Lippincott Williams & Wilkins, 2010, p. 406. ISBN 1-60831-610-6.
- ↑ World Health Organisation. Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008 (PDF). 6th. World Health Organisation, 2011, p. 27. ISBN 978-92-4-150111-8.
- ↑ 92,0 92,1 Berer M «Making abortions safe: a matter of good public health policy and practice». Bull. World Health Organ., vol. 78, 5, 2000, pàg. 580–92. PMC: 2560758. PMID: 10859852.
- ↑ «Translations». Dublin Declaration. [Consulta: 28 octubre 2015].
- ↑ «Induced abortion: estimated rates and trends worldwide». Lancet, vol. 370, 9595, 2007, pàg. 1338–45. DOI: 10.1016/S0140-6736(07)61575-X. PMID: 17933648.
- ↑ 95,0 95,1 «Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003» (PDF). World Health Organization, 2007. Arxivat de l'original el 16 February 2011. [Consulta: 7 març 2011].
- ↑ Berer M «National laws and unsafe abortion: the parameters of change». Reprod Health Matters, vol. 12, 24 Suppl, November 2004, pàg. 1–8. DOI: 10.1016/S0968-8080(04)24024-1. PMID: 15938152.
- ↑ Culwell, Kelly R.; Hurwitz, Manuelle «Addressing barriers to safe abortion». International Journal of Gynecology & Obstetrics, vol. 121, May 2013, pàg. S16–S19. DOI: 10.1016/j.ijgo.2013.02.003.
- ↑ «The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change». BJOG, vol. 112, 3, March 2005, pàg. 355–9. DOI: 10.1111/j.1471-0528.2004.00422.x. PMID: 15713153.
- ↑ Bateman C «Maternal mortalities 90% down as legal TOPs more than triple». S. Afr. Med. J., vol. 97, 12, December 2007, pàg. 1238–42. PMID: 18264602.
- ↑ Conti, Jennifer A.; Brant, Ashley R.; Shumaker, Heather D.; Reeves, Matthew F. «Update on abortion policy». Current Opinion in Obstetrics and Gynecology, November 2016, pàg. 1. DOI: 10.1097/GCO.0000000000000324.
- ↑ New, M. J. «Analyzing the Effect of Anti-Abortion U.S. State Legislation in the Post-Casey Era». State Politics & Policy Quarterly, vol. 11, 1, 15-02-2011, pàg. 28–47. DOI: 10.1177/1532440010387397.
- ↑ Medoff, M. H.; Dennis, C. «Another Critical Review of New's Reanalysis of the Impact of Antiabortion Legislation». State Politics & Policy Quarterly, vol. 14, 3, 21-07-2014, pàg. 269–276. DOI: 10.1177/1532440014535476.
- ↑ «Facts on Investing in Family Planning and Maternal and Newborn Health» (PDF). Guttmacher Institute, 2010. Arxivat de l'original el 24 March 2012. [Consulta: 24 maig 2012].
- ↑ Grimes, David A. «Unsafe Abortion - The Preventable Pandemic*». [Consulta: 16 gener 2010].
- ↑ Nations, MK «Women’s hidden transcripts about abortion in Brazil». Soc Sci Med, vol. 44, 1997, pàg. 1833–45. DOI: 10.1016/s0277-9536(96)00293-6. PMID: 9194245.
- ↑ Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadesIJGO10 - ↑ Error de citació: Etiqueta
<ref>no vàlida; no s'ha proporcionat text per les refs nomenadesDev98-07 - ↑ Maclean, Gaynor. «XI. Dimension, Dynamics and Diversity: A 3D Approach to Appraising Global Maternal and Neonatal Health Initiatives». A: Balin, Randell E.. Trends in Midwifery Research. Nova Publishers, 2005, p. 299–300. ISBN 978-1-59454-477-4.
- ↑ Salter, C. «Care for Postabortion Complications: Saving Women's Lives». Population Reports. Johns Hopkins School of Public Health, vol. 25, 1, 1997.
- ↑ «Packages of interventions: Family planning, safe abortion care, maternal, newborn and child health», 2010. [Consulta: 31 December 2010].
- ↑ «The Care of Women Requesting Induced Abortion. Evidence-Based Clinical Guideline no. 7». Royal College of Obstetricians and Gynaecologists, November 2011 [Consulta: 31 octubre 2015]. «RECOMMENDATION 6.21 Feticide should be performed before medical abortion after 21 weeks and 6 days of gestation to ensure that there is no risk of a live birth.»
- ↑ Society of Family Planning «Clinical Guidelines, Labor induction abortion in the second trimester». Contraception, vol. 84, 1, February 2011, pàg. 4–18. DOI: 10.1016/j.contraception.2011.02.005. «"Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin."»
- ↑ «Fetal intracardiac potassium chloride injection to avoid the hopeless resuscitation of an abnormal abortus: II. Ethical issues.». Obstetrics and Gynecology, vol. 80, 2, Aug 1992, pàg. 310–313. PMID: 1635751. «"... following later abortions at greater than 20 weeks, the rare but catastrophic occurrence of live births can lead to fractious controversy over neonatal management."»
- ↑ «Termination of Pregnancy for Fetal Abnormality». Royal College of Obstetricians and Gynaecologists, May 2010, pàg. 29–31 [Consulta: 26 octubre 2015].
- ↑ Nuffield Council on Bioethics «Critical care decisions in fetal and neonatal medicine: a guide to the report». , 2007 [Consulta: 29 octubre 2015]. «Under English law, fetuses have no independent legal status. Once born, babies have the same rights to life as other people.»
- ↑ «Preterm Birth: Causes, Consequences, and Prevention. C: A Review of Ethical Issues Involved in Premature Birth». Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes;, 2007. «In 2002, the 107th U.S. Congress passed the Born-Alive Infants Protection Act of 2001. This law established personhood for all infants who are born “at any stage of development” who breathe, have a heartbeat, or “definite movement of voluntary muscles,” regardless of whether the birth was due to labor or induced abortion.»
- ↑ Chabot, Steve. «H.R. 2175 (107th): Born-Alive Infants Protection Act of 2002». govtrack.us, 05-08-2002. [Consulta: 30 octubre 2015]. «The term ``born alive is defined as the complete expulsion or extraction from its mother of that member, at any stage of development, who after such expulsion or extraction breathes or has a beating heart, pulsation of the umbilical cord, or definite movement of the voluntary muscles, regardless of whether the umbilical cord has been cut, and regardless of whether the expulsion or extraction occurs as a result of natural or induced labor, cesarean section, or induced abortion.»
- ↑ «Practice Bulletin: Second-Trimester Abortion». Obstetrics & Gynecology, vol. 121, 6, June 2013, pàg. 1394–1406. DOI: 10.1097/01.AOG.0000431056.79334.cc. PMID: 23812485 [Consulta: 30 octubre 2015]. «With medical abortion after 20 weeks of gestation, induced fetal demise may be preferable to the woman or provider in order to avoid transient fetal survival after expulsion.»
- ↑ «Clinical Guidelines: Induction of fetal demise before abortion». Contraception: a publication of Society of Family Planning, vol. 81, January 2010, pàg. 8. DOI: 10.1016/j.contraception.2010.01.018 [Consulta: 26 octubre 2015]. «"Inducing fetal demise before induction termination avoids signs of live birth that may have beneficial emotional, ethical and legal consequences."»
- ↑ Committee on Health Care for Underserved Women «Committee Opinion 613: Increasing Access to Abortion». Obstetrics & Gynecology, vol. 124, November 2014, pàg. 1060–1065. DOI: 10.1097/01.aog.0000456326.88857.31 [Consulta: 28 octubre 2015]. «“Partial-birth” abortion bans—The federal Partial-Birth Abortion Ban Act of 2003 (upheld by the Supreme Court in 2007) makes it a federal crime to perform procedures that fall within the definition of so-called “partial-birth abortion” contained in the statute, with no exception for procedures necessary to preserve the health of the woman...physicians and lawyers have interpreted the banned procedures as including intact dilation and evacuation unless fetal demise occurs before surgery.»
- ↑ «2015 Clinical Policy Guidelines». National Abortion Federation, 2015 [Consulta: 30 octubre 2015]. «Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.»
- ↑ «FIGO (International Federation of Gynecology and Obstetrics) Committee Report: Ethical aspects concerning termination of pregnancy following prenatal diagnosis.». International Journal of Gynecology and Obstetrics, vol. 102, 1, 2008, pàg. 97–98. DOI: 10.1016/j.ijgo.2008.03.002. PMID: 18423641. «"Termination of pregnancy following prenatal diagnosis after 22 weeks must be preceded by a feticide"»
- ↑ «Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015». Centers for Disease Control and Prevention, National Center for Health Statistics [Data are from the Multiple Cause of Death Files, 1999-2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program] [Consulta: 12 novembre 2015].
- ↑ Pazol, Karen «Abortion Surveillance - United States, 2006». Morbidity and Mortality Weekly Report Surveillance Summaries, vol. 58, SS08, 27-11-2009, pàg. 1–35 [Consulta: 12 novembre 2015].
- ↑ Smith Thomas, Heather. «ABORTIONS IN COWS CAN BE CAUSED BY MANY FACTORS» (en anglès). Cattle Today. [Consulta: 30 gener 2016].
- ↑ Tibary, Ahmed. «Abortion in Cattle» (en anglès). The Merck Veterinary Manual, Agost 2015. [Consulta: 30 gener 2016].
- ↑ Tibary, Ahmed. «Abortion in Sheep» (en anglès). The Merck Veterinary Manual, Agost 2015. [Consulta: 2 febrer 2016].
Bibliografia
- Doan, Alesha E. Opposition and Intimidation: The abortion wars and strategies of political harassment. University of Michigan, 2007.
- Ganatra, Bela; Tunçalp, Özge; Johnston, Heidi Bart; Johnson Jr, Brooke R; Gülmezoglu, Ahmet Metin; Temmerman, Marleen «From concept to measurement: operationalizing WHO’s definition of unsafe abortion». Bulletin of the World Health Organization, vol. 92, 3, 01-03-2014, pàg. 155–155. DOI: 10.2471/BLT.14.136333.
- Major, Brenda; et alii. APA Task Force on Mental Health and Abortion. Mental Health and Abortion (pdf) (en anglès). American Psychological Association, 2008, p. 105.
- Sedgh, Gilda; Bearak, Jonathan; Singh, Susheela; Bankole, Akinrinola; Popinchalk, Anna; Ganatra, Bela; Rossier, Clémentine; Gerdts, Caitlin; Tunçalp, Özge «Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends». The Lancet, vol. 388, 10041, July 2016, pàg. 258–267. DOI: 10.1016/S0140-6736(16)30380-4. PMID: 27179755.
- UN. Abortion Policies: A Global Review 3 vols.. Population Division, Department of Economic and Social Affairs, United Nations, 2002.
- WHO. The World Health Report 2005: Make every mother and child count. Geneva: WHO, 2005. ISBN 92 4 156290 0.
- WHO. Safe abortion: technical and policy guidance for health systems. 2nd. Geneva: World Health Organization, 2012. ISBN 9789241548434.
- WHO. «Health worker roles in providing safe abortion care and post-abortion contraception», 2016. [Consulta: 8 gener 2017].
Enllaços externs
| A Wikimedia Commons hi ha contingut multimèdia relatiu a: Avortament |
- Respostes sobre sexualitat per a joves. Generalitat de Catalunya.
- Associació de Planificació Familiar de Catalunya i Balears
- Centre Jove d'Anticoncepció i Sexualitat
